From regional hospital to outpatient centre - escape to the front or rescue in the…

Creating value with Value-based Healthcare: How to get successfully started with outcomes measurement
Our interpretation of Value-based Healthcare (VBHC): what is it, crisp and concise? Despite all the euphoria and excitement around VBHC, Patient-reported outcomes measures (PROMs) and Patient-reported experience measures (PREMs), the implementation of such a transformative approach is challenging. VBHC is a mostly normative concept that lacks a systematic implementation approach. It requires considerable willingness to change. For this reason, our report focuses – on a very practical level – on how to successfully initiate the VBHC-journey and on how to prepare organizations for the overall outcome management. It is based on current client projects in Switzerland and the Netherlands.
An article by Dr. Margot Tanner, Koen Jansen and Francesca Severoni, Consultant at walkerproject.
Methods
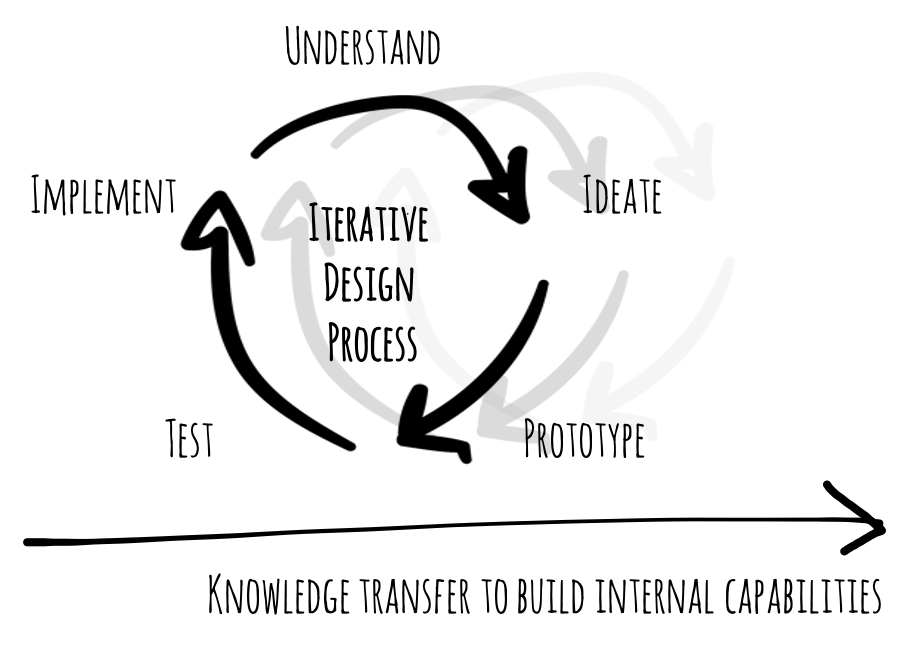
Implementing VBHC is a change process that requires the outmost internal commitment. The buy-in by the physicians and their leadership is crucial. To this end, we adopt Lean methods (e.g. gemba-walks, nemawashi-as-is-analysis1) and follow the Design Thinking (DT) approach. The lean way of implementing sustainable change has proven widely effective in healthcare. DT is considered one of the leading innovation methods for quickly developing innovative solutions that maximize value creation. Key are iterative learning processes and co-creation of prototypes with an interprofessional, hierarchy-spanning project team.
Results
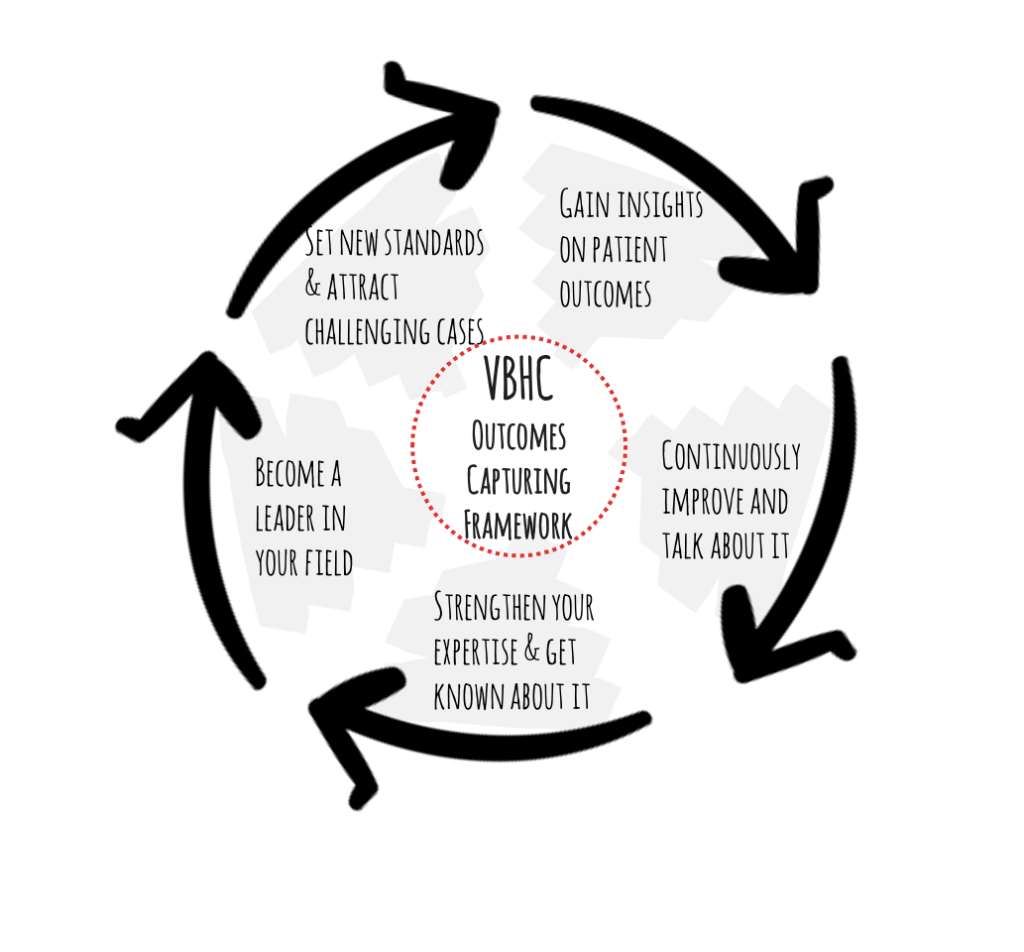
For the VBHC-journey to take off and to get the value generating wheel spinning, the VBHC Outcomes-Capturing-Framework is established. This is the core mechanism for consistently collecting and reporting healthcare outcomes.
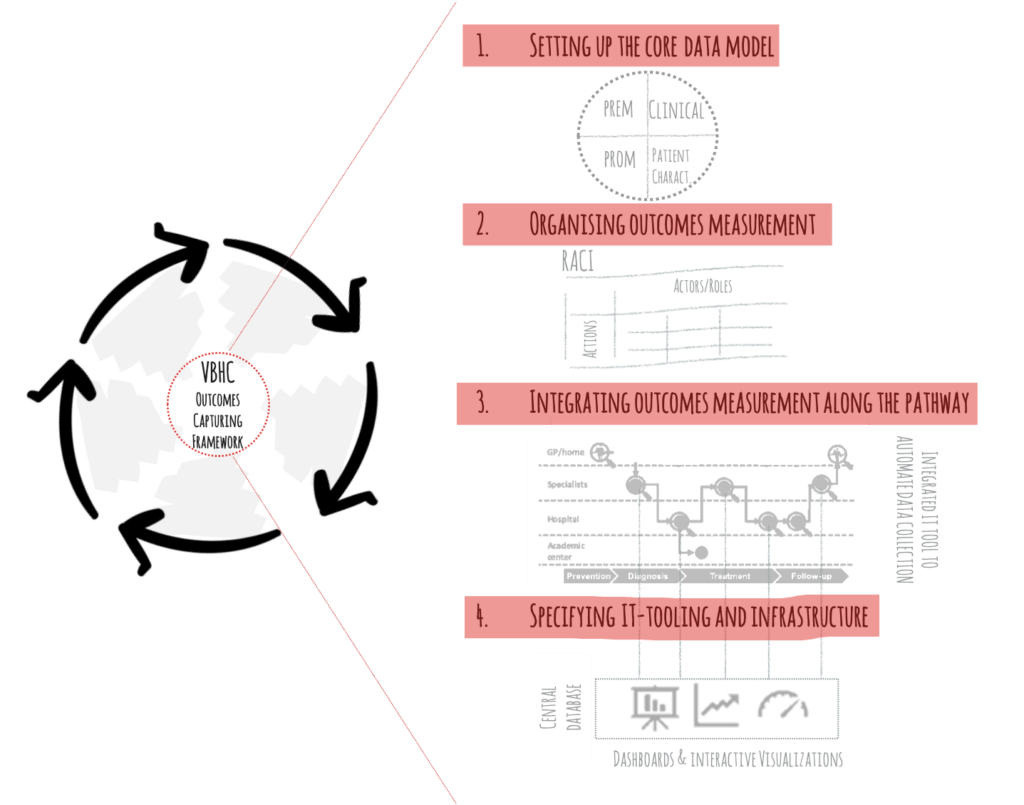
To get started, gemba-walks and a thorough nemawashi-as-is analysis are performed to get a good understanding on how things work today and where the gaps are. Based on these insights, the four main components of the VBHC-Outcomes-Capturing-Framework are prototyped:
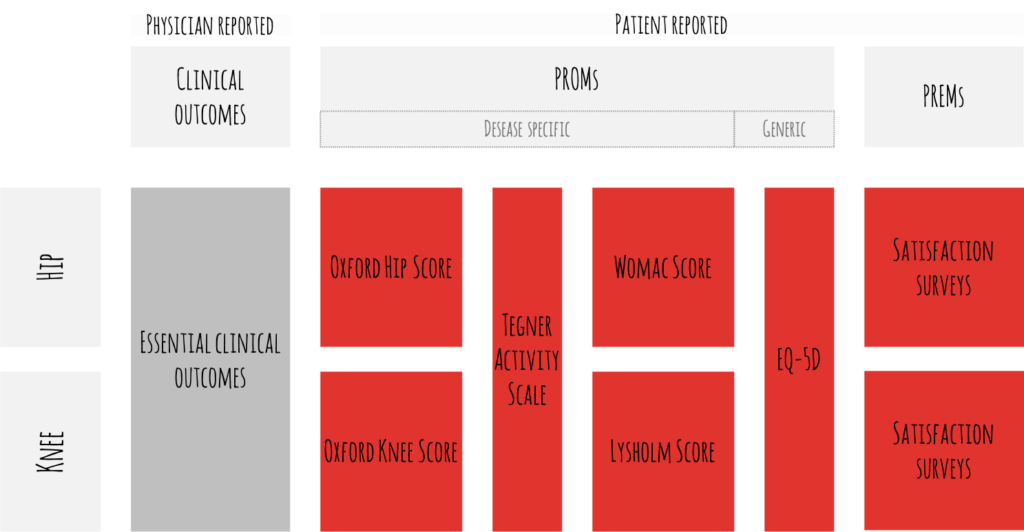
- Setting up the core data model: A consensus is established, and a joint decision taken with the medical team on the relevant input (patient characteristics, health status, treatment variables) and outcome data (clinical outcomes, patient-reported outcomes, process indicators) to be collected.

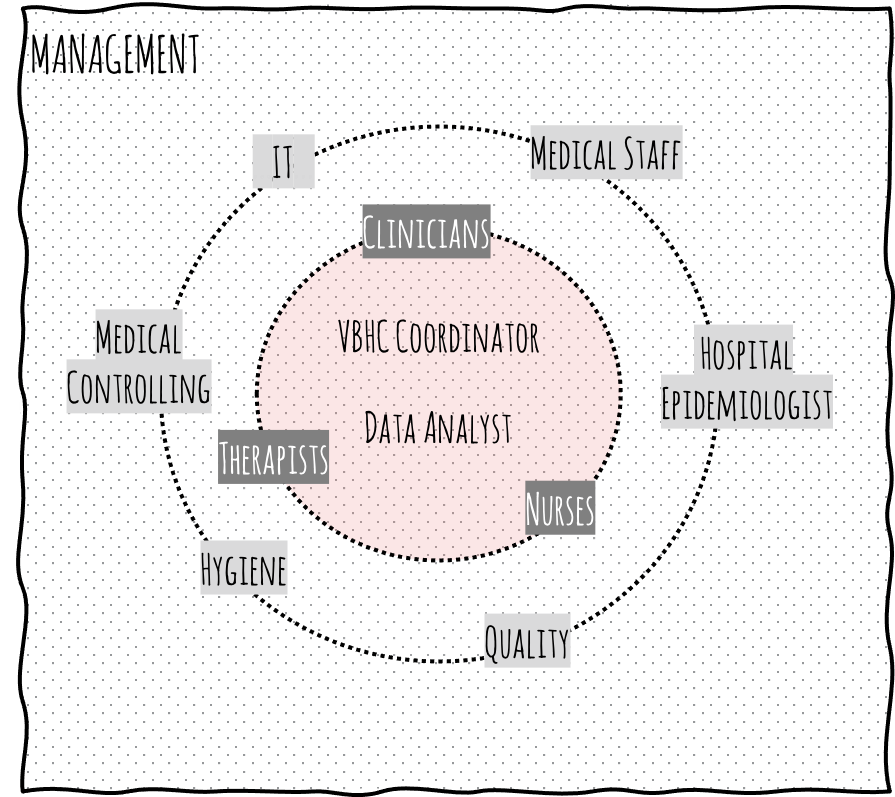
Figure 4: Decide together with the medical and care teams on the outcomes set to be used (generic example for hip and knee) - Organising outcomes measurement: Roles and tasks are defined and assigned to an interprofessional core team. This core team is responsible to collect the VBHC data. Setting-up this team and winning physician leadership is a crucial moment in the VBHC change management.

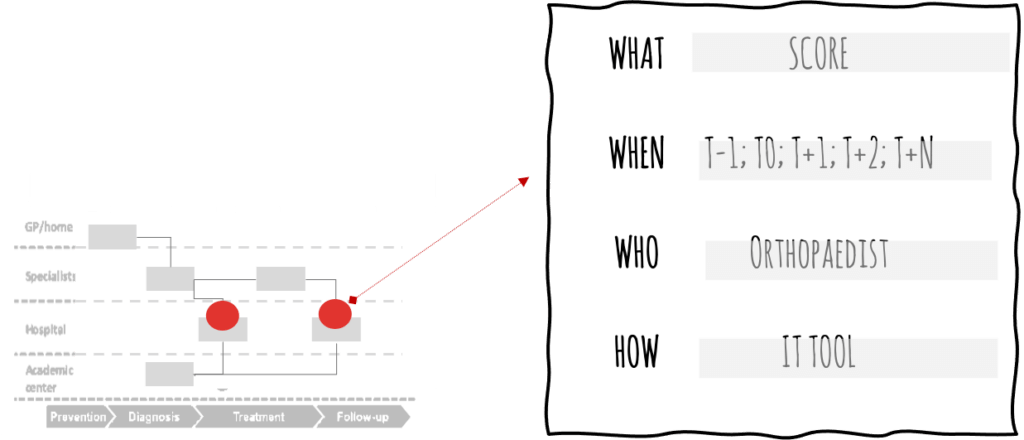
Figure 5: Organising outcomes measurement - Integrating outcomes measurement along the patient-pathway: Based on the as-is insights, the scores are meticulously integrated into the patient-pathway (i.e. which score is collected at what touchpoint, how often, by what method, by whom). Ideally, sub-performing processes are re-engineered at the same time to generate further value.

Figure 6: Mapping & defining touchpoints for outcomes measurements along the patient-pathway - Specifying IT-tooling for outcomes measurements: Often, current data handling is still manual or fragmented in digital siloes. A comprehensive VBHC IT-tool is essential for the smooth and performant outcomes collection, analysis, and reporting. Prototyping the requirements for such an IT tool together with the medical and care staff further strengthens the buy-in by the physicians and their multiprofessional team around them.
Conclusion
Implementing VBHC requires considerable willingness to change. Therefore, paying close attention on what it will bring and how the VBHC-journey gets started is crucial. Developing the VBHC-Outcomes-Capturing-Framework, iteratively with an interprofessional team, is a powerful mechanism to successfully prepare the organisation for the change towards VBHC. Specifically, we have identified five key success factors that facilitate the implementation of VBHC outcomes measurements within medical institutions:
- Clear case for change: Insights gained by the gemba-walks and by the Nemawashi-as-is analysis provide the necessary sense of urgency for change. For example, realizing how fragmented the existing data is across multiple touchpoints motivates actions to streamline processes and to digitize data capturing.
- Dedicated team members, empowered to deliver: The DT approach builds enthusiasm and confidence in the organization.
- Co-creation and engagement: Co-creation leads to stronger interprofessional relationships and collaboration across traditionally siloed entities.
- VBHC knowledge and competence: Along the initial transformational work, the internal project team expands its VBHC competencies and knowledge. This lays the groundwork for self-propelled continuous improvement. It generates the momentum for change management towards VBHC culture and attitude.
- Solid and fast decision making: Maintaining a close working-relationship with a well set-up steering committee, mandated to take decisions throughout the initial phase, helps to stay closely aligned and to quickly move on. It propels their buy-in and guarantees that the strategy is shared by all parties involved. This in turn boosts motivation and willingness to change.